-
传统的肺功能检测仪是基于测量呼气和吸气期间的气流和压力变化来评估受测者的呼吸功能. 这些技术主要基于机械式压差传感器或涡轮传感器, 通过测量受测者口腔吹气和吸气的能力来评估其肺功能. 其所测得的肺功能参数包括峰值呼气流量(peak expiratory flow, PEF)和用力肺活量(forced vital capacity, FVC)等. 本文报道了基于动态湿度传感技术发展而来的穿戴式呼吸功能检测系统(穿戴式呼吸波谱仪). 基于湿度传感器的特点, 对呼吸检测原理与设备的定量设计与模拟潮气实验进行了全面的探索. 根据达西定律, 通过穿戴式呼吸波谱仪的气体流量与其内外压差成正比关系, 该系统符合压差式传感原理. 以此为基础, 根据其结构特点, 建立PEF和FVC与传感器电信号变化的定量关系. 实验结果验证了波谱仪内相对湿度的最大变化率与PEF呈线性正相关的关系. 波谱仪的模拟潮气实验结果表明, 测试范围为180—840 L/min条件下, PEF的示值误差小于10%, 相邻测试误差小于5%, 频率响应测试误差小于12%, 符合呼气峰值流量计行业标准的要求. 此外, 将传统便携式肺功能检测仪作为对照, 进行不同PEF (300—720 L/min)和FVC (3—6 L)条件下的模拟潮气实验. 结果表明, 波谱仪所测PEF和FVC的平均示值误差分别约为0.35%和0.23%, 均远远小于便携式肺功能检测仪, 充分验证了该系统对肺功能实时评估的准确性和可靠性. 更重要的是, 在模拟自由呼吸条件(PEF为12—24 L/min, FVC为0.5—0.7 L)下, 波谱仪的电信号变化与 自由呼吸体积仍呈线性关系. 因此, 穿戴式呼吸波谱仪可对人体自然、微弱的鼻呼吸, 进行自由、动态、定量的长期监测. 所测量人们的自由呼吸波谱在人体肺功能实时监测以及呼吸系统疾病远程监测方面, 具有巨大的应用潜力.
Traditional lung function detectors are based on measuring the changes in airflow and pressure during expiration and inspiration to evaluate the respiratory function of the subject. These techniques are mainly based on mechanical differential pressure sensors or turbine sensors which evaluate the lung function of the subject by measuring the ability of the subject to blow and inhale and determine their lung function parameters, including peak expiratory flow (PEF) and forced vital capacity (FVC). In this study, we present a wearable respiratory function testing system called the wearable respiratory spectrometer, which is developed based on dynamic humidity sensing technology. By exploring the principles and quantitative design of respiratory detection and conducting simulations of humidity sensors, we investigate the comprehensive characteristics of the system. According to Darcy’s law, the gas flow measured by the wearable respiratory spectrometer is directly proportional to the pressure difference inside and outside the device, showing that the system follows the differential pressure sensing principle. According to this basis and combining the structural characteristics of the system, we establish a quantitative relationship among PEF, FVC, and the changes in sensor electrical signals. The experimental results validate a linear positive correlation between the maximum rate of relative humidity change inside the spectrometer and PEF. Additionally, the results of simulated moisture volume experiments of the spectrometer show that in the measurement range from 180 to 840 L/min, the indication error of PEF is less than 10%, the adjacent test error is less than 5%, and the frequency response test error is less than 12%, which meet the industry standards for peak expiratory flow meters. Moreover, we compare the spectrometer with traditional portable lung function testing devices in simulated moisture volume experiments at different PEFs (300 to 720 L/min) and FVCs (3 to 6 L) . The results demonstrate that the average indication error of measured PEF and FVC by the spectrometer are about 0.35% and 0.23%, respectively, both are much lower than those of the portable lung function testing devices, thus fully verifying the accuracy and reliability of this system for real-time lung function assessment. Importantly, under simulated free-breathing conditions (PEF from 12 to 24 L/min, FVC from 0.5 to 0.7 L), the changes in the electrical signals of the spectrometer maintain a linear relationship with the moisture volume. Therefore, the wearable respiratory spectrometer can provide the long-term, free, dynamic, and quantitative monitoring of natural and weak nasal breathing. The measured respiratory spectra of subjects have great potential in real-time monitoring of lung function and remote monitoring of respiratory system diseases. [1] Guillamet R V, Ursu O, Iwamoto G, Moseley P L, Oprea T 2018 Health Inform. J. 24 394
 Google Scholar
Google Scholar
[2] Kostikas K, Gogali A, Hillas G 2023 Am. J. Respir. Crit. Care Med. 208 502
 Google Scholar
Google Scholar
[3] Pelkonen M 2008 Curr. Opin. Pulm. Med. 14 105
 Google Scholar
Google Scholar
[4] Trivedi D 2020 Prim. Health Care Res. 21 e41
 Google Scholar
Google Scholar
[5] 殷鹏, 王黎君, 刘世炜, 刘韫宁, 刘江美, 由金玲, 曾新颖, 周脉耕 2015 中华预防医学杂志 49 364
 Google Scholar
Google Scholar
Yin P, Wang L J, Liu S W, Liu Y N, Liu J M, You J L, Zeng X Y, Zhou M G 2015 Chin. J. Prev. Med. 49 364
 Google Scholar
Google Scholar
[6] 中华医学会呼吸病学分会慢性阻塞性肺疾病学组, 中国医师协会呼吸医师分会慢性阻塞性肺疾病工作委员会 2020 中华结核和呼吸杂志 43 421
 Google Scholar
Google Scholar
Chronic Obstructive Pulmonary Disease Group of Chinese Thoracic Society Chronic, Obstructive Pulmonary Disease Committee of Chinese Association of Chest Physician 2020 Chin. J. Tuberc. Respir. Dis. 43 421
 Google Scholar
Google Scholar
[7] Sode B F, Dahl M, Nordestgaard B G 2011 Eur. Heart J. 32 2365
 Google Scholar
Google Scholar
[8] Hassoun P M 2021 New Engl. J. Med. 385 2361
 Google Scholar
Google Scholar
[9] Stanojevic S, Kaminsky D A, Miller M R, Thompson B, Aliverti A, Barjaktarevic I, Cooper B G, Culver B, Derom E, Hall G L, Hallstrand T S, Leuppi J D, MacIntyre N, McCormack M, Rosenfeld M, Swenson E R 2022 Eur. Respir. J. 60 2101499
 Google Scholar
Google Scholar
[10] Reese J T, Blau H, Casiraghi E, Bergquist T, Loomba J J, Callahan T J, Laraway B, Antonescu C, Coleman B, Gargano M, Wilkins K J, Cappelletti L, Fontana T, Ammar N, Antony B, Murali T M, Caufield J H, Karlebach G, McMurry J A, Williams A, Moffitt R, Banerjee J, Solomonides A E, Davis H, Kostka K, Valentini G, Sahner D, Chute C G, Madlock-Brown C, Haendel M A, Robinson P N, Consortium N C, Consortium R 2023 Ebiomedicine 87 104413
 Google Scholar
Google Scholar
[11] Cao Y, Wang J, Jian F, Xiao T, Song W, Yisimayi A, Huang W, Li Q, Wang P, An R, Wang Y, Niu X, Yang S, Liang H, Sun H, Li T, Yu Y, Cui Q, Liu S, Yang X, Du S, Zhang Z, Hao X, Shao F, Jin R, Wang X, Xiao J, Wang Y, Xie X S 2022 Nature 602 657
 Google Scholar
Google Scholar
[12] Zhang Y, Aniruddha P, Hou C, Lu D, Qiu W, Kong L, Wu R, Ma L, Yu R, Yu W, Liu X Y 2022 Chem. Eng. J. 428 132362
 Google Scholar
Google Scholar
[13] Zhang Y, Chen C, Qiu Y, Ma L, Qiu W, Yu R, Yu W, Liu X Y 2021 Adv. Funct. Mater. 31 2100150
 Google Scholar
Google Scholar
[14] Wu R, Ma L, Liu X Y 2022 Adv. Sci. 9 e2103981
 Google Scholar
Google Scholar
[15] Shi C, Hu F, Wu R, Xu Z, Shao G, Yu R, Liu X Y 2021 Adv. Mater. 33 e2005910.
 Google Scholar
Google Scholar
[16] He F, You X, Gong H, Yang Y, Bai T, Wang W, Guo W, Liu X, Ye M 2020 ACS Appl. Mater. Interfaces 12 6442
 Google Scholar
Google Scholar
[17] Huang J, Xu Z, Qiu W, Chen F, Meng Z, Hou C, Guo W, Liu X Y 2020 Adv. Funct. Mater. 30 1910547
 Google Scholar
Google Scholar
[18] Ma L, Patil A, Wu R, Zhang Y, Meng Z, Zhang W, Kong L, Liu X Y, Wang J 2021 Nanotechnology 32 19lt01
 Google Scholar
Google Scholar
[19] Tu H, Yu R, Lin Z, Zhang L, Lin N, Yu W D, Liu X Y 2016 Adv. Funct. Mater. 26 9032
 Google Scholar
Google Scholar
[20] Zhu S, Zeng W, Meng Z, Luo W, Ma L, Li Y, Lin C, Huang Q, Lin Y, Liu X Y 2019 Adv. Mater. 31 1900870
 Google Scholar
Google Scholar
[21] Lin N, Liu X Y 2015 Chem. Soc. Rev. 44 7881
 Google Scholar
Google Scholar
[22] Jiao C L, Shao G W, Chen Y Y, Liu X Y 2023 Chin. Phys. B 32 038103
 Google Scholar
Google Scholar
[23] Meng F B, Sana B, Li Y G, Liu Y J, Lim S, Chen X D 2014 Small 10 277
 Google Scholar
Google Scholar
[24] Moin A, Zhou A, Rahimi A, Menon A, Benatti S, Alexandrov G, Tamakloe S, Ting J, Yamamoto N, Khan Y, Burghardt F, Benini L, Arias A C, Rabaey J M 2021 Nat. Electron. 4 54
[25] Zhang W, Liu X, Lin Y, Ma L, Kong L, Min G, Wu R, Mengane S K, Yang L, Patil A B, Liu X Y 2022 Chin. Phys. B 31 028201
 Google Scholar
Google Scholar
[26] Hu F, Li W, Zou M, Li Y, Chen F, Lin N, Guo W, Liu X Y 2020 ACS Nano 15 9559
 Google Scholar
Google Scholar
[27] Diao Y Y, Liu X Y, Toh G W, Shi L, Zi J 2013 Adv. Funct. Mater. 23 5373
 Google Scholar
Google Scholar
[28] Moser B, Bodrogi F, Eibl G, Lechner M, Rieder J, Lirk P 2005 Respir. Physiol. Neurobiol. 145 295
 Google Scholar
Google Scholar
[29] Smolinska A, Baranska A, Dallinga J W, Mensink R P, Baumgartner S, van de Heijning B J, Mvan Schooten F J 2019 Sci. Rep. 9 554
 Google Scholar
Google Scholar
[30] Ma L, Liu Q, Wu R, Meng Z, Patil A, Yu R, Yang Y, Zhu S, Fan X, Hou C, Li Y, Qiu W, Huang L, Wang J, Lin N, Wan Y, Hu J, Liu X Y 2020 Small 16 2000203
 Google Scholar
Google Scholar
[31] Ma L, Wu R, Patil A, Zhu S, Meng Z, Meng H, Hou C, Zhang Y, Liu Q, Yu R, Wang J, Lin N, Liu X Y 2019 Adv. Funct. Mater. 29 1904549
 Google Scholar
Google Scholar
[32] YY/T 1438-2016 麻醉和呼吸设备评价 自主呼吸者肺功能的呼气峰值流量 (北京: 中国标准出版社)
YY/T 1438-2016 Anaesthetic and Respiratory Equipment— Peak Expiratory Flow Meters for the Assessment of Pulmonary Function in Spontaneously Breathing Humans (Beijing: Standards Press of China
[33] Hayashi T, Sano Y, Shigematsu H, Sugimoto R, Sakao N, Sakaue T 2019 J. Thorac. Oncol. 14 S601
 Google Scholar
Google Scholar
[34] Ikonen T, Harjula A L J, Kinnula V L, Savola J, Sovijarvi A 1995 J. Heart Lung Transpl. 14 244
[35] Nolan K M, Dornelly S M, Hughes D T, Strunin L 1992 Respir. Med. 86 525
 Google Scholar
Google Scholar
[36] Donahue J F 2016 COPD 3 512
 Google Scholar
Google Scholar
[37] Zhang X, Zhang X, Taira H, Liu H 2019 J. Power Sources 412 391
 Google Scholar
Google Scholar
[38] Gao X, Li T, Meng N, Gao H, Li X, Gao R, Wang Z, Wang J 2023 Renewable Energy 206 428
 Google Scholar
Google Scholar
[39] Siegel A C, Phillips S T, Dickey M D, Lu N, Suo Z, Whitesides G M 2010 Adv. Funct. Mater. 20 28
 Google Scholar
Google Scholar
[40] Wang W, Chen T, Li Z, Tan Q, Meng Z, Qiu H, Liu X, Zheng J 2022 Am. J Infect. Control 50 516
 Google Scholar
Google Scholar
[41] Ma L, Pan C, Teng Y, Shangguan Z 2013 Earth Surf. Processes Landforms 38 1523
 Google Scholar
Google Scholar
[42] Rengasamy S, Shaffer R, Williams B, Smit S 2017 J. Occup. Environ. Hyg. 14 92
 Google Scholar
Google Scholar
[43] Pan J, Harb C, Leng W, Marr L C 2021 Aerosol Sci. Technol. 55 718
 Google Scholar
Google Scholar
[44] Jia X Y, Wang X R, Jiang Y Y, An M Z, Pei D Q, Li Z P, Zhou Q H 2023 Minerva Anestesiol. 89 762
 Google Scholar
Google Scholar
[45] Li T, Divatia S, McKittrick J, Moss J, Hijnen N M, Becker L B 2019 Open access Emergency Med. 11 103
 Google Scholar
Google Scholar
[46] Lovett P B, Buchwald J M, Stürmann K, Bijur P 2005 Ann. Emergency Med. 45 68
 Google Scholar
Google Scholar
-
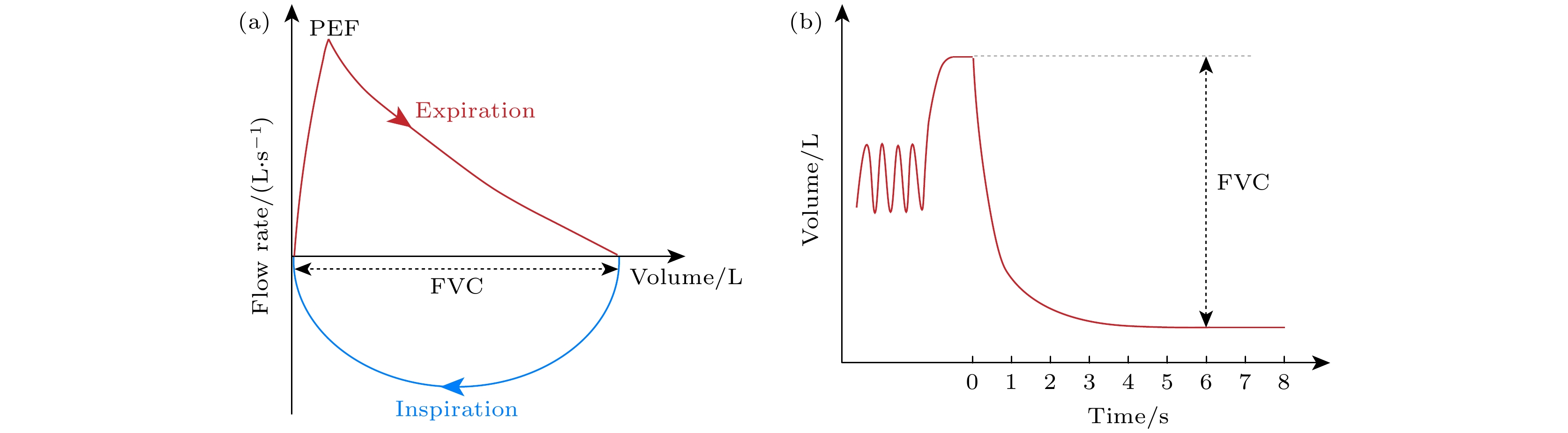
图 1 用力呼气测试获取肺功能参数的曲线示意图 (a)呼气流量-容积曲线, 用于描述个体在呼气(或吸气)过程中的气流速度与容积变化之间的关系; (b)呼气容积-时间曲线, 通过测量个体在一段时间内的呼气(或吸气)流量和相应的容积来获得
Fig. 1. Schematic diagram of the curve of pulmonary function parameters obtained by forced exhalation test: (a) The expiratory flow-volume curve is used to describe the relationship between the airflow velocity and volume changes of an individual during exhalation (or inhalation); (b) the expiratory volume-time curve is used to measure the individual’s time during a period of time. The expiratory or inspiratory flow rate and corresponding volume within the time period are obtained.
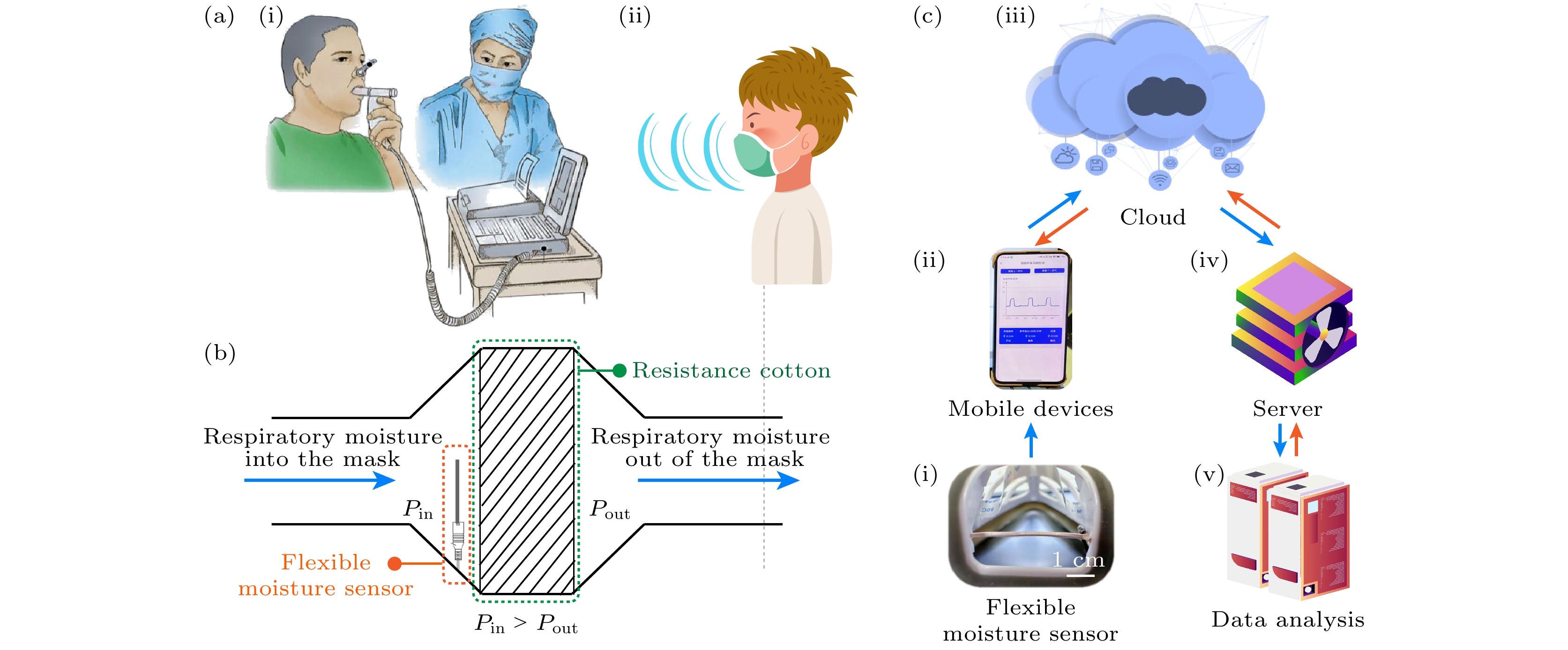
图 2 穿戴式呼吸波谱仪的呼吸功能检测与测定原理及其全系统的示意图 (a)肺功能检测过程, 其中(i)传统肺功能检测仪只能采取从嘴用力呼出气的形式, 同时需要专业医护人员在场指导; (ii)基于动态湿度传感技术的穿戴式呼吸波谱仪可以对嘴呼吸和鼻呼吸进行定量检测和监测, 保证受测者正常呼吸的同时, 设备也方便穿戴. (b)穿戴式呼吸波谱仪定量测定人体呼吸原理示意图. 以呼气过程为例, 呼气过程人体呼吸潮气进入穿戴式呼吸波谱仪, 穿戴式呼吸波谱仪内潮气含量与气体压力均增大. 在此压差下, 穿戴式呼吸波谱仪内潮气通过阻力棉离开其内部. 此过程符合达西定律, 即潮气的体积流速与穿戴式呼吸波谱仪内外水蒸气的分压差成正比; (c)基于动态湿度传感技术的穿戴式呼吸波谱仪系统, 其中(i) 动态湿度传感器, 将人体呼吸过程的潮气变化定量的转化为的电信号; (ii)移动端应用软件, 建立与穿戴式呼吸波谱仪的实时连接; (iii)云平台, 通过手机将数据实时发送至云端后台; (iv)服务器与(v)数据处理与分析, 对原始电信号进行定量分析、计算以及储存
Fig. 2. Respiratory function detection and measurement principle of the wearable respiratory spectrometer and the schematic diagram of the entire system. (a) Pulmonary function testing process: (i) Traditional pulmonary function testing instruments can only take the form of exhaling forcefully from the mouth, and require professional medical staff to be present for guidance; (ii) a wearable respiratory spectrometer based on dynamic sensing technology can mouth breathing and nasal breathing are quantitatively detected and monitored to ensure that the subject breathes normally while the device is also easy to wear. (b) Schematic diagram of the principle of quantitative measurement of human respiration by a wearable respiratory spectrometer. Take the exhalation process as an example. During the exhalation process, human respiratory moisture enters the wearable respiratory spectrometer, and the moisture content and gas pressure in the wearable respiratory spectrometer increase. Under this pressure difference, the moisture in the wearable respiratory spectrometer leaves its interior through the resistance cotton. This process complies with the Darcy’s law, that is, the volumetric flow rate of moisture is directly proportional to the partial pressure difference of water vapor inside and outside the wearable respiratory spectrometer. (c) The wearable respiratory spectrometer system based on dynamic humidity sensing technology includes. (i) Dynamic humidity sensor: Quantitatively converts the moisture changes during human breathing into electrical signals. (ii) Mobile application software: Established and worn real-time connection of respiratory spectrometer. (iii) Cloud platform: Send data to the cloud backend in real time through mobile phone. (iv) Server and (v) data analysis: Perform quantitative analysis, calculation and storage of original electrical signals.
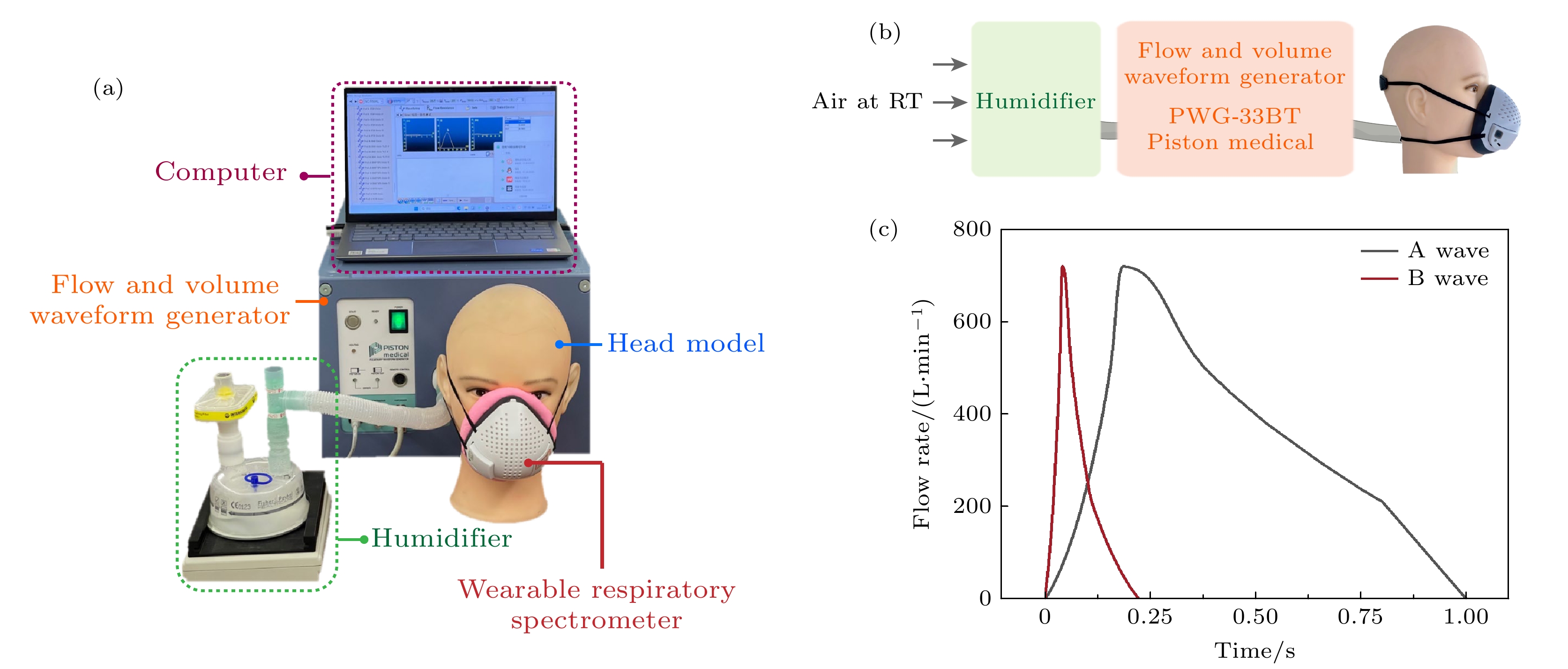
图 3 呼吸波模拟器测试 (a)呼吸波模拟器测试系统照片; (b) 测试过程中, 模拟潮气的流通路径示意图; (c)呼吸波模拟器所输出的波形为行标[32]所规定的A波形和B波形, 模拟潮气体积流速随时间的变化关系
Fig. 3. Flow and volume waveform generator testing: (a) Photo of the flow and volume waveform generator test system; (b) schematic diagram of the flow path of simulated moisture during the testing process; (c) the waveform output by the flow and volume waveform generator is the A waveform and B waveform specified in the industry standard “YY/T 1438-2016”[32] to simulate the change of flow rate of respiratory moisture with time.
图 5 穿戴式呼吸波谱仪内相对湿度最大变化率与潮气的体积流速的定量关系. 结果表明, 穿戴式呼吸波谱仪内相对湿度最大变化率与峰值呼气流量PEF呈线性相关(R2 = 0.9993)
Fig. 5. Quantitative relationship between the maximum change rate of relative humidity $ {\mathrm{M}}{\mathrm{a}}{\mathrm{x}}({\mathrm{d}}\eta /{\mathrm{d}}t) $ in the wearable respiratory spectrometer and PEF. The results show that $ {\mathrm{M}}{\mathrm{a}}{\mathrm{x}}({\mathrm{d}}\eta /{\mathrm{d}}t) $ is linearly related to PEF (R2 = 0.9993).
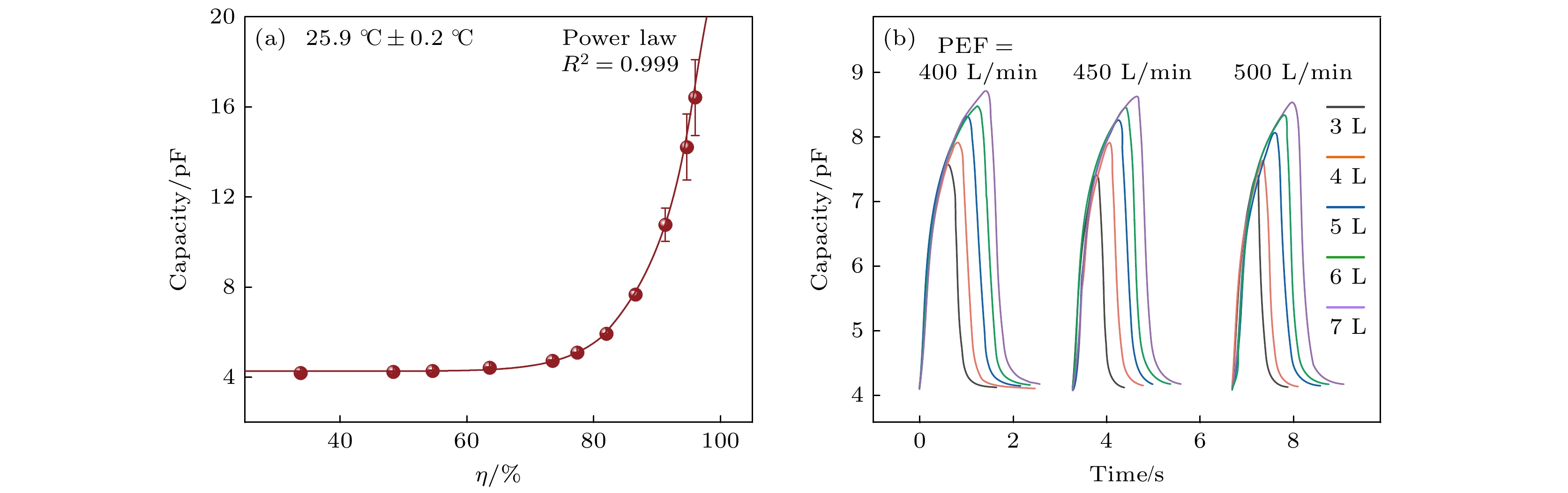
图 4 基于电容型湿度传感器的穿戴式呼吸波谱仪用于呼吸定量监测 (a)湿度传感器电容和环境相对湿度的关系. 实验结果表明, 湿度传感器电信号强度即电容值随着湿度的增加而增加, 符合(6)式幂函数关系; (b)使用呼吸波模拟器研究穿戴式呼吸波谱仪内湿度传感器电容值与潮气的峰值流速PEF和呼气体积FVC的关系. 实验结果表明, 电信号变化强度随呼气体积的增大而增大. 不同PEF下, 同一FVC电信号变化强度基本相同
Fig. 4. Wearable respiratory spectrometer based on the capacitive flexible moisture sensor is used for quantitative respiratory monitoring: (a) The relationship between the capacitance of the flexible moisture sensor and the relative humidity of the environment. Experimental results show that the electrical signal strength of the flexible moisture sensor, that is, the capacitance value, increases with the increase in humidity, consistent with the power function relationship of Eq. (6); (b) use a flow and volume waveform generator to study the capacitance value of the flexible moisture sensor in a wearable respiratory spectrometer relationship to PEF and FVC. Experimental results show that the intensity of changes in electrical signals increases with the increase in FVC. Under different PEF, the intensity of changes in the electrical signal for the same expiration volume is basically the same.
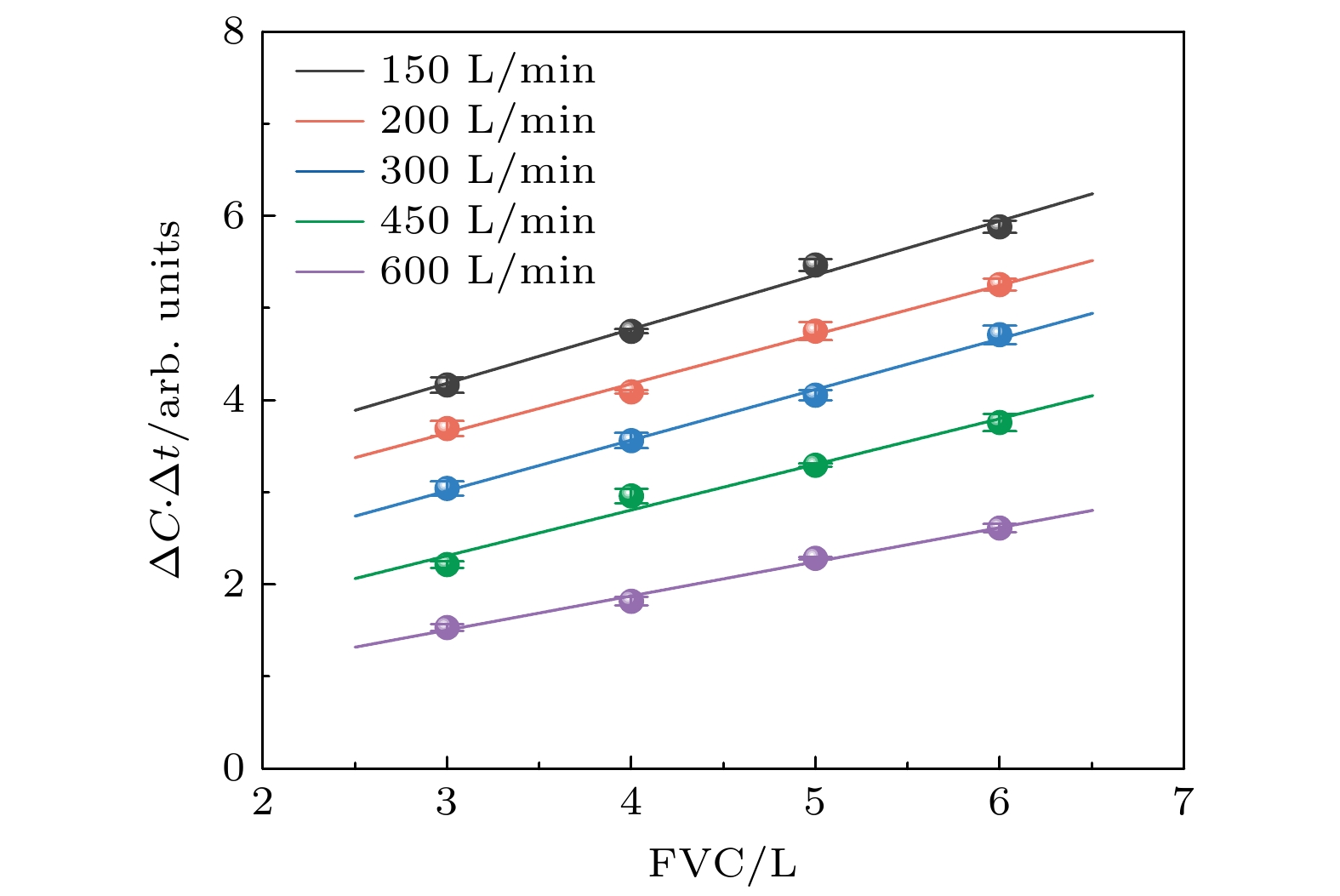
图 6 穿戴式呼吸波谱仪传感电信号变化与潮气的体积(FVC)的定量关系. 结果表明, 潮气体积与电信号变化和呼气时间的乘积成正比, 因此可根据传感器电信号变化确定呼吸量
Fig. 6. Quantitative relationship between the changes in electrical signals sensed by the wearable respiratory spectrometer and FVC. The results show that FVC is proportional to the product of the electrical signal change and the expiration time, so the respiratory volume can be determined based on the sensor electrical signal change.
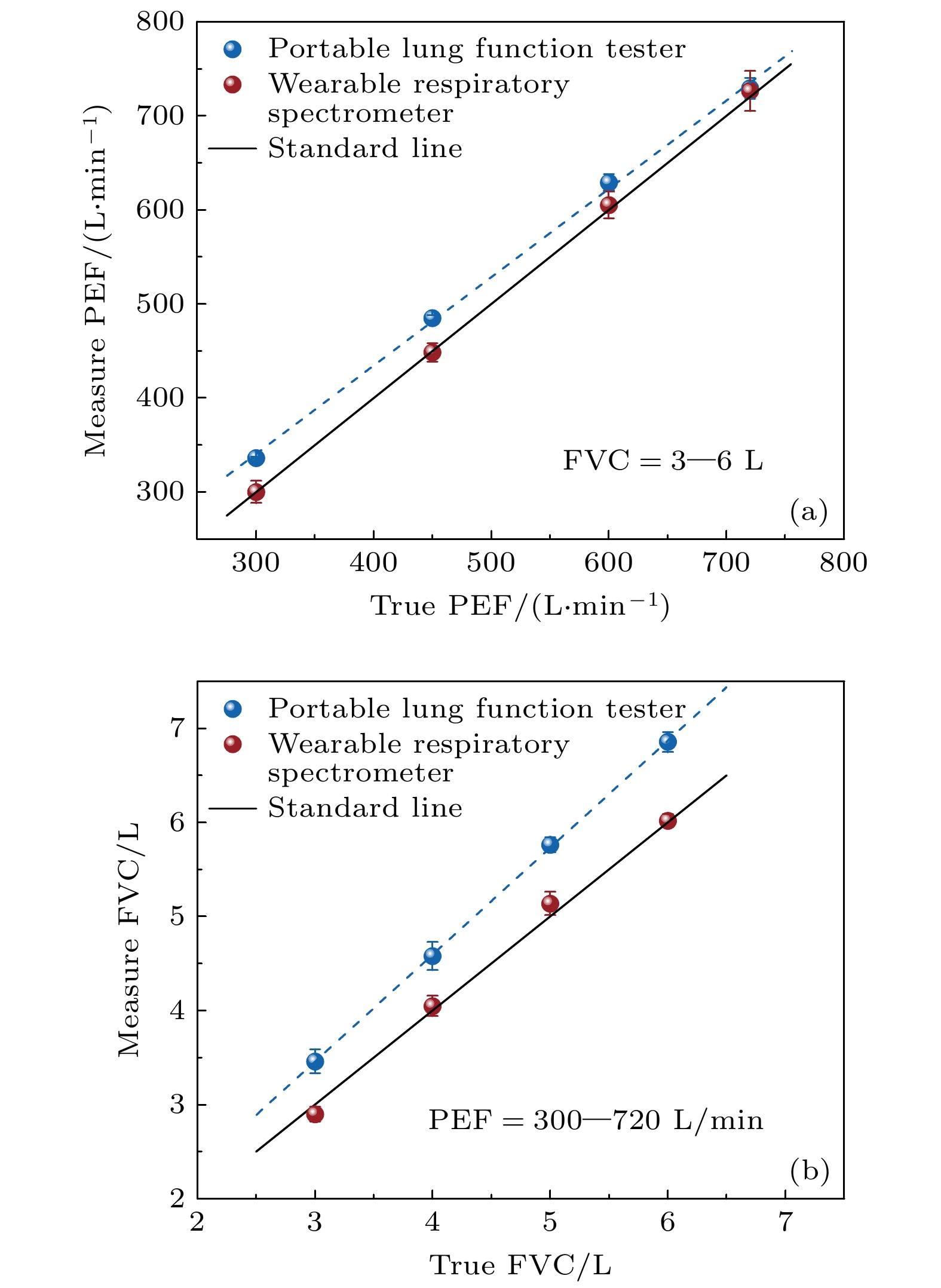
图 7 穿戴式呼吸波谱仪与市售肺功能检测仪(肺活量计B1, 广州红象医疗科技有限公司)的用力呼气测试结果 (a) PEF和(b) FVC的对比. 结果表明, 在所采取测试条件下, 穿戴式呼吸波谱仪具有与市面上肺功能检测仪相当的, 甚至更加优异的准确度
Fig. 7. Comparison of forced expiration test results: (a) PEF and (b) FVC between a wearable respiratory spectrometer and a commercial pulmonary function tester (Vitality Meter B1, Guangzhou Hongxiang Medical Technology Co., Ltd). The results show that under the test conditions adopted, the wearable respiratory spectrometer has an accuracy comparable to or even better than that of lung function testers on the market.
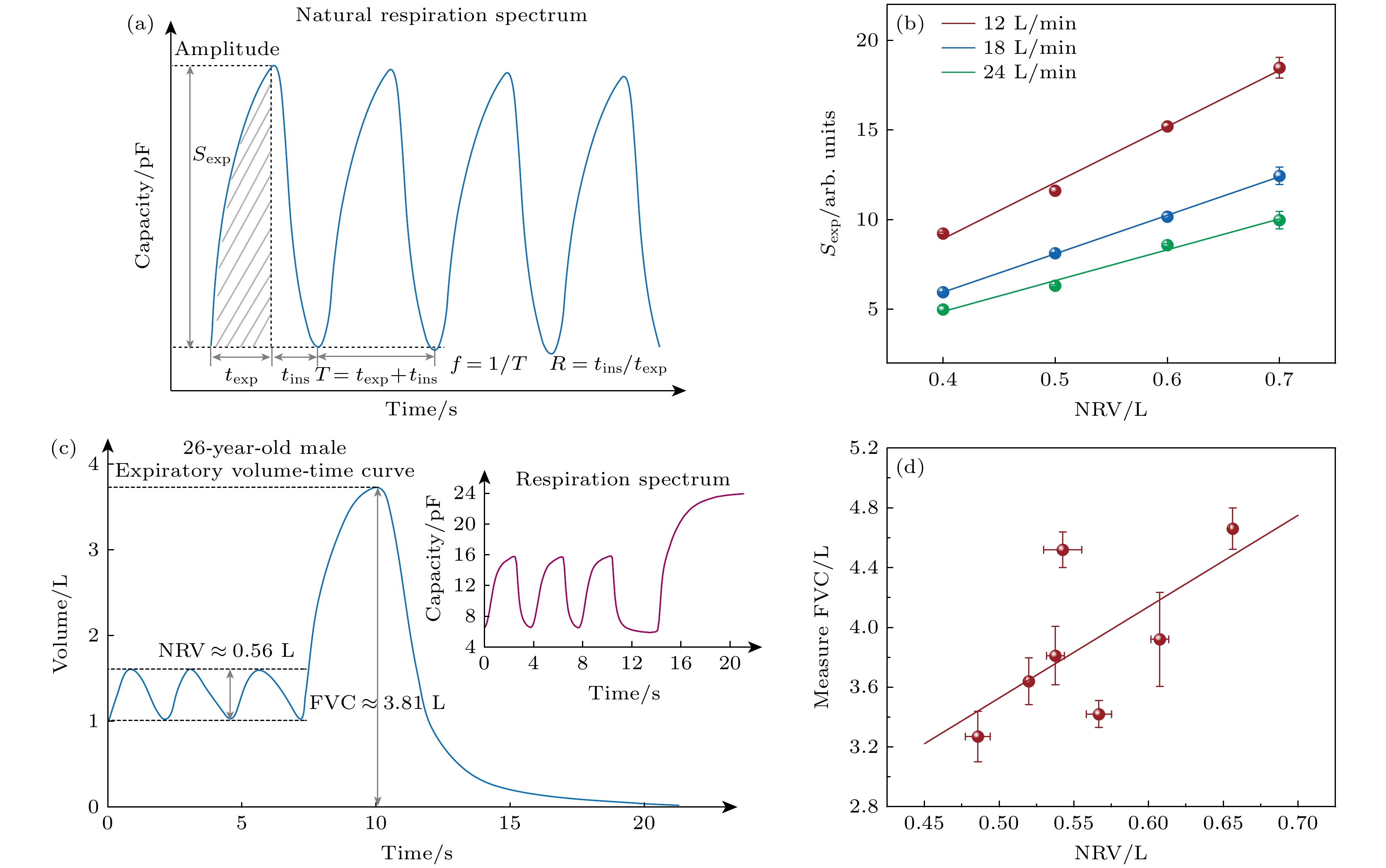
图 8 穿戴式呼吸波谱仪通过自由呼吸对肺功能进行监测 (a)通过穿戴式呼吸波谱仪获得的自由呼吸图谱及其相关物理量的定量定义. 吸气时间tins和呼气时间texp之比为吸呼比R, 两者之和为一个自由呼吸周期TR. 自由呼吸周期TR内, 呼吸波的波峰和波谷的差值定义为呼吸幅度, 其值在数值上等于电信号变化量$ {{\Delta }}C $, 自由呼吸频率fR为呼吸周期TR的倒数. 呼吸波曲线呼气段与曲线最低点所围成的面积定义为Sexp, 其值可用$ {{\Delta }}C $与$ {{\Delta }}t $的乘积估计; (b) 模拟自由呼吸情况下, Sexp与NRV成线性关系; (c)通过穿戴式呼吸波谱仪获得的自由呼吸过程和用力呼气过程的呼吸量与时间的变化曲线(右上插入图为呼吸图谱, 即电信号随时间的变化曲线); (d) 穿戴式呼吸波谱仪获得的健康志愿者的NRV与FVC的关系, 结果表明NRV与FVC基本成正相关, 可作为肺功能评估的重要指标
Fig. 8. Wearable respiratory spectrometer monitors lung function through natural respiration: (a) Quantitative definition of the natural respiration spectrum obtained by the wearable respiratory spectrometer and its related physical quantities. The ratio of the inhalation time tins and the expiration time texp is the inhalation-to-exhalation ratio (R), and the sum of the two is a natural respiration cycle time (TR). During the natural respiration period TR, the difference between the peak and the trough of the respiratory wave is defined as the respiratory amplitude, and its value is numerically equal to the electrical signal change amount ΔC. The natural respiration frequency (fR) is the reciprocal of TR. The area enclosed by the expiratory segment of the respiratory wave curve and the lowest point of the curve is defined as Sexp, and its value can be estimated by the product of ΔC and Δt; (b) under simulated natural respiration, Sexp has a linear relationship with NRV; (c) the expiratory volume-time curve of the natural respiration process and the forced exhalation process obtained through the wearable respiratory spectrometer (inserted is the respiratory spectrum, that is, the change curve of the electrical signal with time); (d) the relationship between the natural respiration volume (NRV) and FVC measured by the wearable respiratory spectrometer of healthy volunteers. The results show that NRV and FVC are basically positively correlated and can be used as an important indicator for lung function assessment.
表 1 示值误差、相邻测试误差和频率响应误差测试结果*
Table 1. Indication error, adjacent test error and frequency response error test results*.
实际峰值流量 A波形第n次测试值 n+1次测试值 B波形测试值 示值误差 相邻测试 频率响应测试 PEFreal/(L·min–1) PEFtest/(L·min–1) PEFn+1/(L·min–1) PEFB/(L·min–1) <10% 误差<5% 误差<12% 180 180.9 177.8 182.5 0.4% 0.9% 1.8% 360 359.8 355.9 360.4 0.6% 0.5% 0.7% 540 544.7 557.4 539.8 2.0% 1.2% 2.0% 600 591.6 621.5 — 1.1% 2.5% — 720 713.5 746.7 — 1.4% 2.3% — 840 834.7 830.9 — 0.9% 0.2% — *表1中示值误差、相邻误差和频率响应误差的测试仅展示一次测试结果作为示例, 实际上5次平行测试结果均符合误差要求. -
[1] Guillamet R V, Ursu O, Iwamoto G, Moseley P L, Oprea T 2018 Health Inform. J. 24 394
 Google Scholar
Google Scholar
[2] Kostikas K, Gogali A, Hillas G 2023 Am. J. Respir. Crit. Care Med. 208 502
 Google Scholar
Google Scholar
[3] Pelkonen M 2008 Curr. Opin. Pulm. Med. 14 105
 Google Scholar
Google Scholar
[4] Trivedi D 2020 Prim. Health Care Res. 21 e41
 Google Scholar
Google Scholar
[5] 殷鹏, 王黎君, 刘世炜, 刘韫宁, 刘江美, 由金玲, 曾新颖, 周脉耕 2015 中华预防医学杂志 49 364
 Google Scholar
Google Scholar
Yin P, Wang L J, Liu S W, Liu Y N, Liu J M, You J L, Zeng X Y, Zhou M G 2015 Chin. J. Prev. Med. 49 364
 Google Scholar
Google Scholar
[6] 中华医学会呼吸病学分会慢性阻塞性肺疾病学组, 中国医师协会呼吸医师分会慢性阻塞性肺疾病工作委员会 2020 中华结核和呼吸杂志 43 421
 Google Scholar
Google Scholar
Chronic Obstructive Pulmonary Disease Group of Chinese Thoracic Society Chronic, Obstructive Pulmonary Disease Committee of Chinese Association of Chest Physician 2020 Chin. J. Tuberc. Respir. Dis. 43 421
 Google Scholar
Google Scholar
[7] Sode B F, Dahl M, Nordestgaard B G 2011 Eur. Heart J. 32 2365
 Google Scholar
Google Scholar
[8] Hassoun P M 2021 New Engl. J. Med. 385 2361
 Google Scholar
Google Scholar
[9] Stanojevic S, Kaminsky D A, Miller M R, Thompson B, Aliverti A, Barjaktarevic I, Cooper B G, Culver B, Derom E, Hall G L, Hallstrand T S, Leuppi J D, MacIntyre N, McCormack M, Rosenfeld M, Swenson E R 2022 Eur. Respir. J. 60 2101499
 Google Scholar
Google Scholar
[10] Reese J T, Blau H, Casiraghi E, Bergquist T, Loomba J J, Callahan T J, Laraway B, Antonescu C, Coleman B, Gargano M, Wilkins K J, Cappelletti L, Fontana T, Ammar N, Antony B, Murali T M, Caufield J H, Karlebach G, McMurry J A, Williams A, Moffitt R, Banerjee J, Solomonides A E, Davis H, Kostka K, Valentini G, Sahner D, Chute C G, Madlock-Brown C, Haendel M A, Robinson P N, Consortium N C, Consortium R 2023 Ebiomedicine 87 104413
 Google Scholar
Google Scholar
[11] Cao Y, Wang J, Jian F, Xiao T, Song W, Yisimayi A, Huang W, Li Q, Wang P, An R, Wang Y, Niu X, Yang S, Liang H, Sun H, Li T, Yu Y, Cui Q, Liu S, Yang X, Du S, Zhang Z, Hao X, Shao F, Jin R, Wang X, Xiao J, Wang Y, Xie X S 2022 Nature 602 657
 Google Scholar
Google Scholar
[12] Zhang Y, Aniruddha P, Hou C, Lu D, Qiu W, Kong L, Wu R, Ma L, Yu R, Yu W, Liu X Y 2022 Chem. Eng. J. 428 132362
 Google Scholar
Google Scholar
[13] Zhang Y, Chen C, Qiu Y, Ma L, Qiu W, Yu R, Yu W, Liu X Y 2021 Adv. Funct. Mater. 31 2100150
 Google Scholar
Google Scholar
[14] Wu R, Ma L, Liu X Y 2022 Adv. Sci. 9 e2103981
 Google Scholar
Google Scholar
[15] Shi C, Hu F, Wu R, Xu Z, Shao G, Yu R, Liu X Y 2021 Adv. Mater. 33 e2005910.
 Google Scholar
Google Scholar
[16] He F, You X, Gong H, Yang Y, Bai T, Wang W, Guo W, Liu X, Ye M 2020 ACS Appl. Mater. Interfaces 12 6442
 Google Scholar
Google Scholar
[17] Huang J, Xu Z, Qiu W, Chen F, Meng Z, Hou C, Guo W, Liu X Y 2020 Adv. Funct. Mater. 30 1910547
 Google Scholar
Google Scholar
[18] Ma L, Patil A, Wu R, Zhang Y, Meng Z, Zhang W, Kong L, Liu X Y, Wang J 2021 Nanotechnology 32 19lt01
 Google Scholar
Google Scholar
[19] Tu H, Yu R, Lin Z, Zhang L, Lin N, Yu W D, Liu X Y 2016 Adv. Funct. Mater. 26 9032
 Google Scholar
Google Scholar
[20] Zhu S, Zeng W, Meng Z, Luo W, Ma L, Li Y, Lin C, Huang Q, Lin Y, Liu X Y 2019 Adv. Mater. 31 1900870
 Google Scholar
Google Scholar
[21] Lin N, Liu X Y 2015 Chem. Soc. Rev. 44 7881
 Google Scholar
Google Scholar
[22] Jiao C L, Shao G W, Chen Y Y, Liu X Y 2023 Chin. Phys. B 32 038103
 Google Scholar
Google Scholar
[23] Meng F B, Sana B, Li Y G, Liu Y J, Lim S, Chen X D 2014 Small 10 277
 Google Scholar
Google Scholar
[24] Moin A, Zhou A, Rahimi A, Menon A, Benatti S, Alexandrov G, Tamakloe S, Ting J, Yamamoto N, Khan Y, Burghardt F, Benini L, Arias A C, Rabaey J M 2021 Nat. Electron. 4 54
[25] Zhang W, Liu X, Lin Y, Ma L, Kong L, Min G, Wu R, Mengane S K, Yang L, Patil A B, Liu X Y 2022 Chin. Phys. B 31 028201
 Google Scholar
Google Scholar
[26] Hu F, Li W, Zou M, Li Y, Chen F, Lin N, Guo W, Liu X Y 2020 ACS Nano 15 9559
 Google Scholar
Google Scholar
[27] Diao Y Y, Liu X Y, Toh G W, Shi L, Zi J 2013 Adv. Funct. Mater. 23 5373
 Google Scholar
Google Scholar
[28] Moser B, Bodrogi F, Eibl G, Lechner M, Rieder J, Lirk P 2005 Respir. Physiol. Neurobiol. 145 295
 Google Scholar
Google Scholar
[29] Smolinska A, Baranska A, Dallinga J W, Mensink R P, Baumgartner S, van de Heijning B J, Mvan Schooten F J 2019 Sci. Rep. 9 554
 Google Scholar
Google Scholar
[30] Ma L, Liu Q, Wu R, Meng Z, Patil A, Yu R, Yang Y, Zhu S, Fan X, Hou C, Li Y, Qiu W, Huang L, Wang J, Lin N, Wan Y, Hu J, Liu X Y 2020 Small 16 2000203
 Google Scholar
Google Scholar
[31] Ma L, Wu R, Patil A, Zhu S, Meng Z, Meng H, Hou C, Zhang Y, Liu Q, Yu R, Wang J, Lin N, Liu X Y 2019 Adv. Funct. Mater. 29 1904549
 Google Scholar
Google Scholar
[32] YY/T 1438-2016 麻醉和呼吸设备评价 自主呼吸者肺功能的呼气峰值流量 (北京: 中国标准出版社)
YY/T 1438-2016 Anaesthetic and Respiratory Equipment— Peak Expiratory Flow Meters for the Assessment of Pulmonary Function in Spontaneously Breathing Humans (Beijing: Standards Press of China
[33] Hayashi T, Sano Y, Shigematsu H, Sugimoto R, Sakao N, Sakaue T 2019 J. Thorac. Oncol. 14 S601
 Google Scholar
Google Scholar
[34] Ikonen T, Harjula A L J, Kinnula V L, Savola J, Sovijarvi A 1995 J. Heart Lung Transpl. 14 244
[35] Nolan K M, Dornelly S M, Hughes D T, Strunin L 1992 Respir. Med. 86 525
 Google Scholar
Google Scholar
[36] Donahue J F 2016 COPD 3 512
 Google Scholar
Google Scholar
[37] Zhang X, Zhang X, Taira H, Liu H 2019 J. Power Sources 412 391
 Google Scholar
Google Scholar
[38] Gao X, Li T, Meng N, Gao H, Li X, Gao R, Wang Z, Wang J 2023 Renewable Energy 206 428
 Google Scholar
Google Scholar
[39] Siegel A C, Phillips S T, Dickey M D, Lu N, Suo Z, Whitesides G M 2010 Adv. Funct. Mater. 20 28
 Google Scholar
Google Scholar
[40] Wang W, Chen T, Li Z, Tan Q, Meng Z, Qiu H, Liu X, Zheng J 2022 Am. J Infect. Control 50 516
 Google Scholar
Google Scholar
[41] Ma L, Pan C, Teng Y, Shangguan Z 2013 Earth Surf. Processes Landforms 38 1523
 Google Scholar
Google Scholar
[42] Rengasamy S, Shaffer R, Williams B, Smit S 2017 J. Occup. Environ. Hyg. 14 92
 Google Scholar
Google Scholar
[43] Pan J, Harb C, Leng W, Marr L C 2021 Aerosol Sci. Technol. 55 718
 Google Scholar
Google Scholar
[44] Jia X Y, Wang X R, Jiang Y Y, An M Z, Pei D Q, Li Z P, Zhou Q H 2023 Minerva Anestesiol. 89 762
 Google Scholar
Google Scholar
[45] Li T, Divatia S, McKittrick J, Moss J, Hijnen N M, Becker L B 2019 Open access Emergency Med. 11 103
 Google Scholar
Google Scholar
[46] Lovett P B, Buchwald J M, Stürmann K, Bijur P 2005 Ann. Emergency Med. 45 68
 Google Scholar
Google Scholar
计量
- 文章访问数: 9396
- PDF下载量: 595
- 被引次数: 0












 下载:
下载: