-
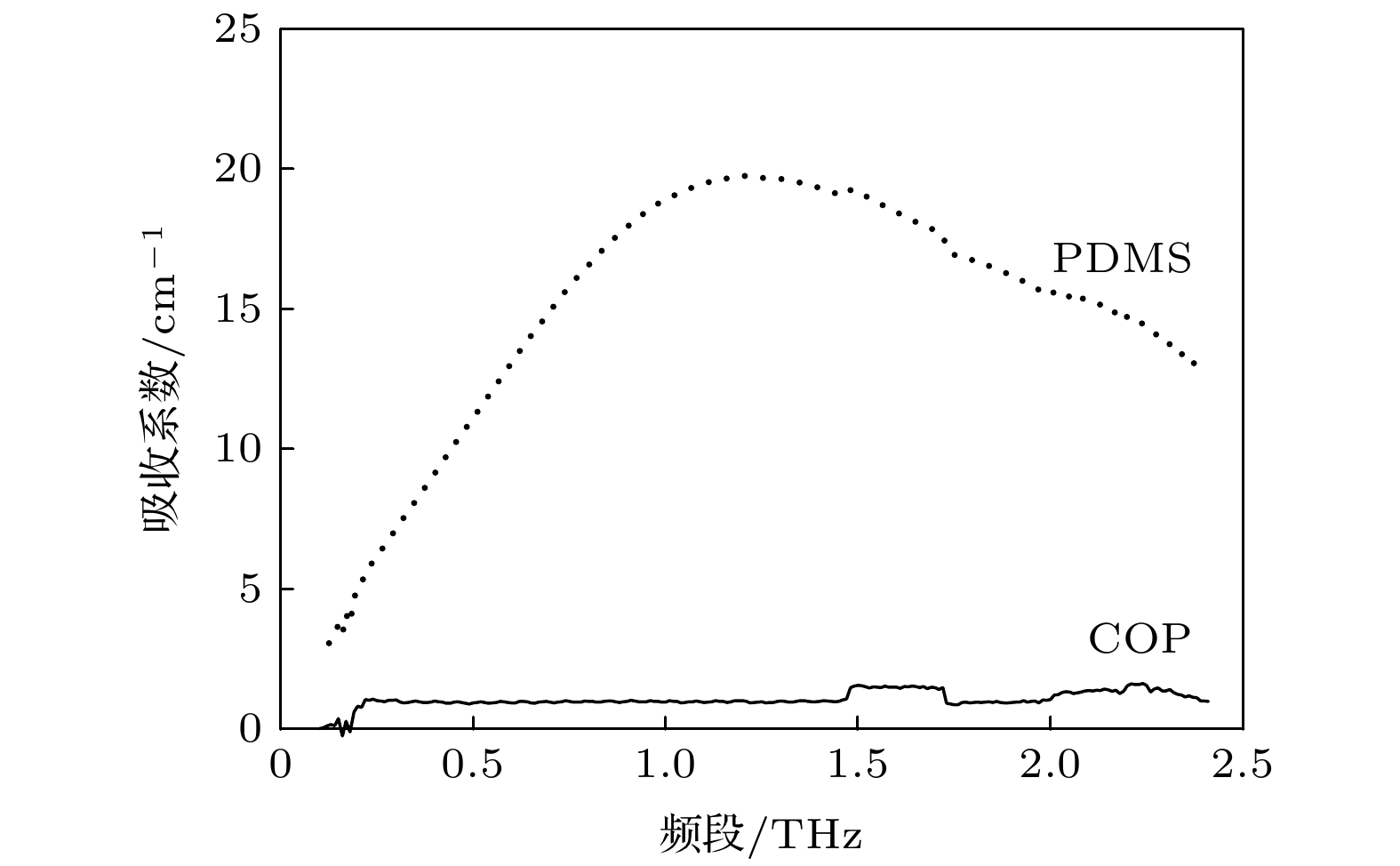
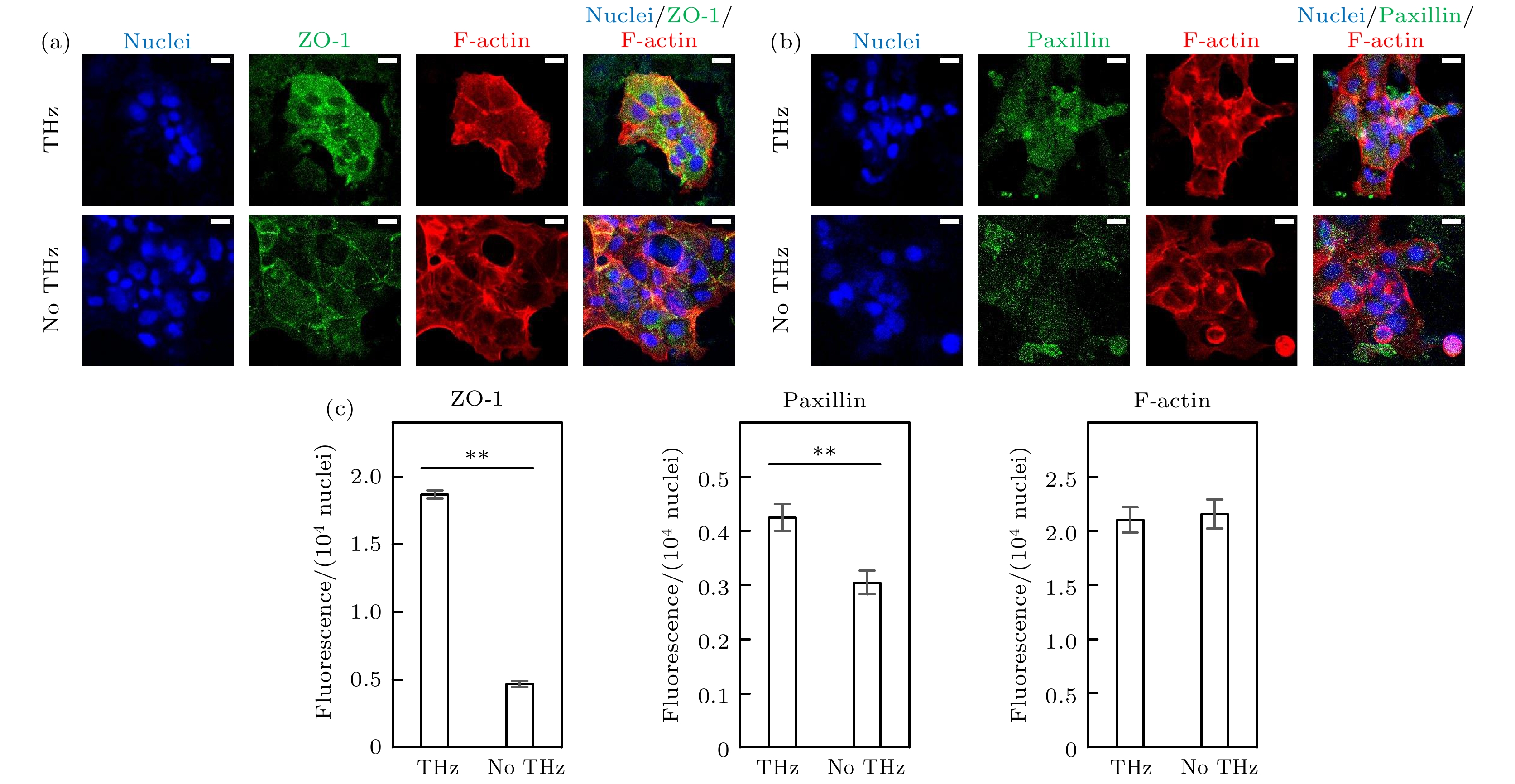
用于细胞培养的常规培养皿无法直接用于激光共聚焦显微镜的观察, 在很大程度上限制了细胞水平上的太赫兹生物效应研究的开展. 本文采用了对太赫兹吸收率低的材料—环烯烃聚合物(COP), 与聚二甲基硅氧烷(PDMS)进行共键合, 借用软蚀刻、光刻、等离子清洗和高温高压孵育技术将两种材料整合成新型微流控芯片, 并利用该微流控芯片探索太赫兹对肠道细胞的生物效应. 该微流控芯片可实现肠上皮细胞Caco-2的动态培养, 原位免疫荧光染色及激光共聚焦显微镜的直接观察, 为太赫兹细胞水平的生物效应研究提供了高效便捷的实验环境. 研究中将微流控芯片中培养的肠上皮细胞Caco-2经15 mW/cm2 的0.1 THz波辐照10 min, 免疫荧光染色结果显示细胞贴附生长的形态改变, 胞间紧密连接蛋白ZO-1及桩蛋白Paxillin的水平及分布发生变化, 提示太赫兹对细胞的胞外连接及胞间连接均可产生影响, 可减弱细胞与培养界面的黏附. 本研究设计制备的COP-PDMS共键合微流控芯片为探索太赫兹对细胞的生物效应提供了便捷有效的平台, 有望在未来进一步用于太赫兹对细胞分子效应的实时研究.
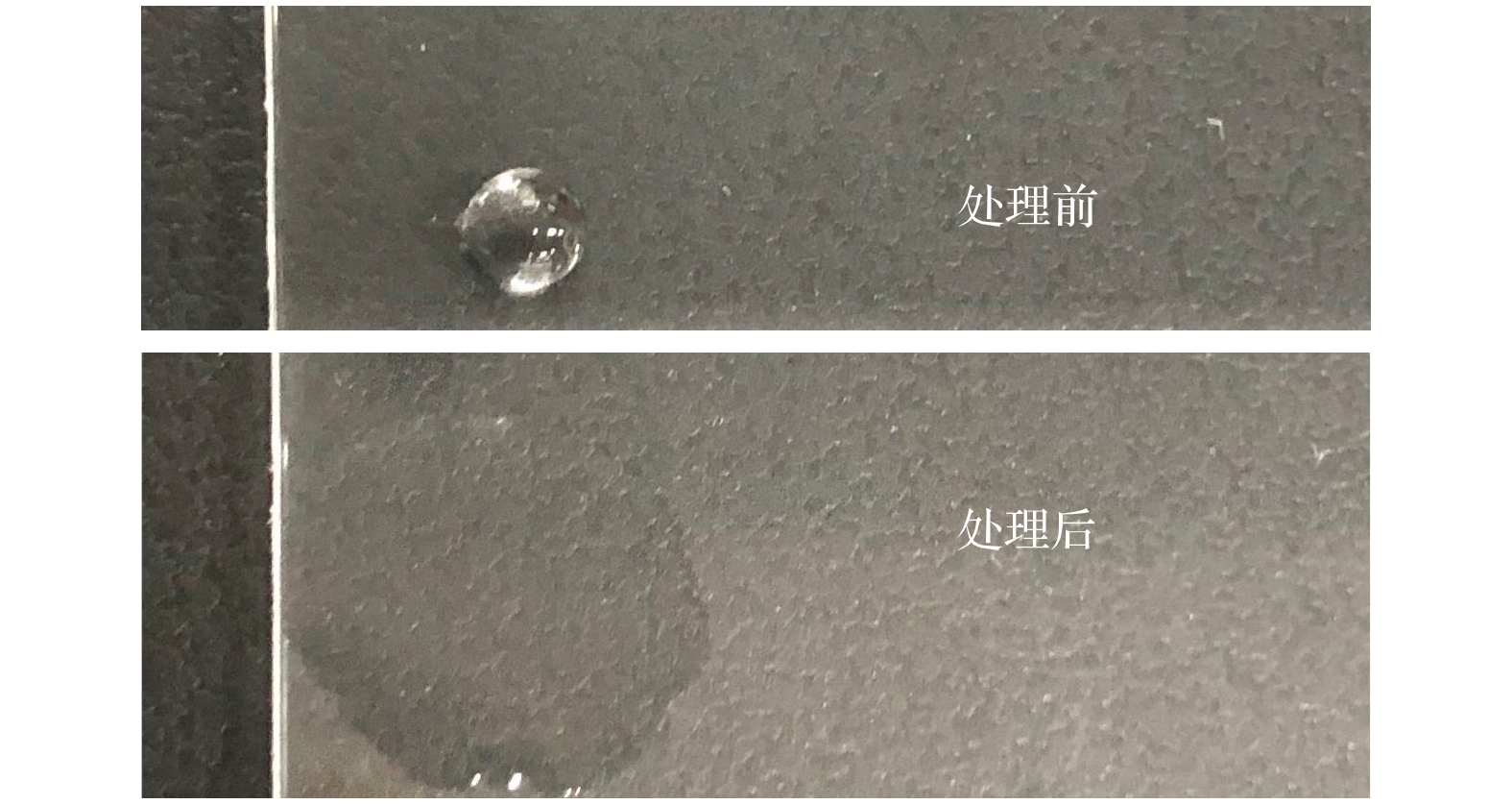
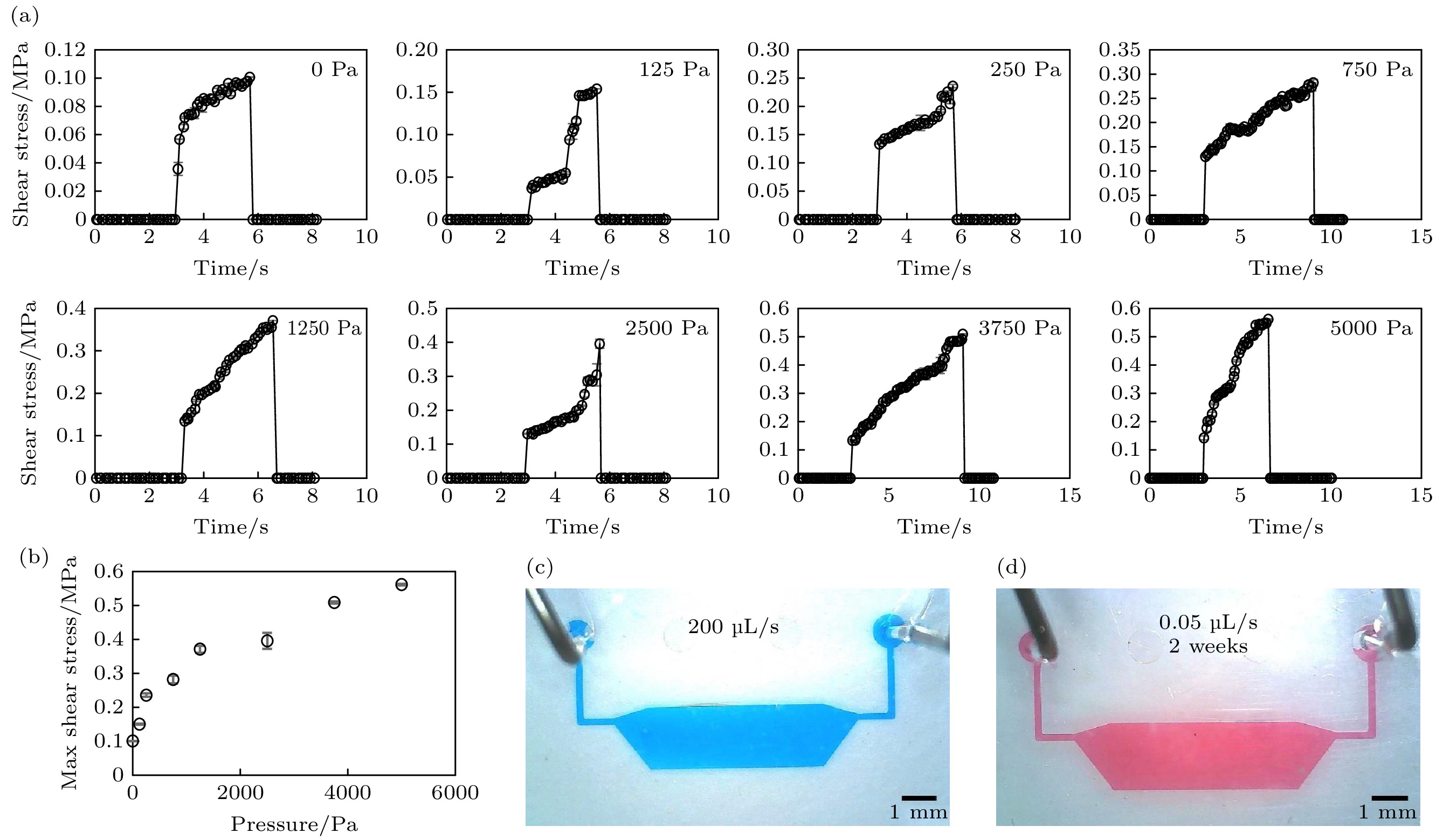
The current research on the terahertz biological effects at a cellular level is limited by the conventional petri dishes used for cell culture, which cannot be directly used for confocal laser microscopy. In this research, the cycloolefin polymer (COP), a material that possesses low terahertz absorption rate but excellent optical property for microscopy, is bonded to polydimethylsiloxane (PDMS), thereby developing a novel COP-PDMS microfluidic device by using the techniques of soft etching, photolithography, plasma cleaning, high-temperature and high-pressure incubation. The bonding strength of resulting device is tested by using a push-tension meter. The results indicate that the developed device shows a bonding strength as strong as the device fabricated by quartz and PDMS, which is thought as the tightest binding in the multiple types of microfluidic device. In addition, by perfusing the device chamber at a high flow rate (200 μL/s) and long-term time-course (2 weeks), which simulates the dynamic shearing stress occurring in in-vivo organs and tissues, this COP-PDMS microfluidic device can still maintain the original shape and sealing property, indicating that this device qualifies the requirements of the following dynamic cell culture. The biological effects of terahertz on the cells are explored by using this COP-PDMS microfluidic device mentioned above. In this device, we develop the dynamic culture of intestinal epithelial cells Caco-2 with a perfusion rate of 0.05 μL/s, which meets the findings of the in-vivo gastrointestinal lumen shearing stress. The Caco-2 cells are then irradiated with 0.1 THz wave with the power of 15 mW/cm2 for 3 days, and the irradiation duration is 10 min per day. The biological effects of terahertz irradiation on the intercellular tight junction protein ZO-1, the Paxillin relating to the cell adhesion and migration, and the cytoskeletal microfilament protein F-actin of Caco-2 cells are detected in the device directly using the technique of immunofluorescence staining. The results show that the morphology of cell adhesion as well as the level and distribution of ZO-1 and Paxillin are changed. In brief, the protein expression of ZO-1 and Paxillin are induced more by the terahertz irradiation, while the F-actin is not influenced by the irradiation. As can be seen from the F-actin results, the cells without terahertz irradiation show a spread and outward shape with regular smooth cell edge while a contraction and burr shape of cell edge are shown after irradiation, suggesting that the cell adhesion is weakened after irradiation. Even though the expression level of F-actin is consistent, the changed morphology indicates that terahertz may regulate the interaction and aggregation among actin proteins in cells. Interestingly, the ZO-1 presents diffuse distribution in the cells and its location on the cell membrane is not obvious, that is, a large amount of ZO-1 expresses not only on the cell membrane but also in the intracellular matrix after the irradiation. The expression of Paxillin is enhanced after terahertz irradiation, and some cells show local aggregation and distribution of Paxillin. These indicate that the terahertz irradiation might affect the biomolecular mechanism of synthesis and distribution of protein. The COP-PDMS co-bonded microfluidic device developed in this study provides a convenient and effective platform for exploring the biological effects of terahertz irradiation on cells, and is expected to be further used for real-time research on the effects of terahertz on cells and molecules in the future. [1] Fröhlich H 1975 Proc. Natl. Acad. Sci. U. S. A. 72 4211
 Google Scholar
Google Scholar
[2] Smye S W, Chamberlain J M, Fitzgerald A J, Berry E 2001 Phys. Med. Biol. 46 R101
 Google Scholar
Google Scholar
[3] Qin J, Ying Y, Xie L 2013 Appl. Spectrosc. Rev. 48 439
 Google Scholar
Google Scholar
[4] Greschner A A, Ropagnol X, Kort M, Zuberi N, Perreault J, Razzari L, Ozaki T, Gauthier M A 2019 J. Am. Chem. Soc. 141 3456
 Google Scholar
Google Scholar
[5] Yamazaki S, Harata M, Idehara T, Konagaya K, Yokoyama G, Hoshina H, Ogawa Y 2018 Sci. Rep. 8 9990
 Google Scholar
Google Scholar
[6] Titova L V, Ayesheshim A K, Golubov A, Fogen D, Rodriguez-Juarez R, Hegmann F A, Kovalchuk O 2013 Biomed. Opt. Express 4 559
 Google Scholar
Google Scholar
[7] Olshevskaya J S, Kozlov A, Petrov A K, Zapara T A, Ratushnyak A 2010 Vestn. Novosib. State Univ. Ser. Phys. 5 185
[8] Alfihed S, Holzman J F, Foulds I G 2020 Biosens. Bioelectron. 165 112393
 Google Scholar
Google Scholar
[9] Naftaly M, Gregory A 2021 Appl. Sci. 11 6733
 Google Scholar
Google Scholar
[10] Cunningham P, Valdes N, Vallejo F, Hayden L, Polishak B, Zhou X H, Luo J, Jen A, Williams J, Twieg R 2011 J. Appl. Phys. 109 043505
 Google Scholar
Google Scholar
[11] Alfihed S, Bergen M H, Ciocoiu A, Holzman J F, Foulds I G 2018 Micromachines-Basel 9 E453
 Google Scholar
Google Scholar
[12] Cheng C, Zhu Z, Li S, Ren G, Zhang J, Cong H, Peng Y, Han J, Chang C, Zhao H 2019 RSC Adv. 9 20240
 Google Scholar
Google Scholar
[13] George P A, Hui W, Rana F, Hawkins B G, Smith A E, Kirby B J 2008 Opt. Express 16 1577
 Google Scholar
Google Scholar
[14] Wang C, Dang T, Baste J, Joshi A A, Bhushan A 2021 FASEB J. 35 e21291
 Google Scholar
Google Scholar
[15] Wang C, Tanataweethum N, Karnik S, Bhushan A 2018 ACS Biomater. Sci. Eng. 4 1377
 Google Scholar
Google Scholar
[16] Xu B Y, Yan X N, Xu J J, Chen H Y 2012 Biomicrofluidics 6 16507
 Google Scholar
Google Scholar
[17] Jang K J, Mehr A P, Hamilton G A, McPartlin L A, Chung S, Suh K Y, Ingber D E 2013 Integr. Biol. 5 1119
 Google Scholar
Google Scholar
[18] Kim S W, Ehrman J, Ahn M R, Kondo J, Lopez A A M, Oh Y S, Kim X H, Crawley S W, Goldenring J R, Tyska M J, Rericha E C, Lau K S 2017 Mol. Biol. Cell 28 3043
 Google Scholar
Google Scholar
[19] D'Angelo F, Mics Z, Bonn M, Turchinovich D 2014 Opt. Express 22 12475
 Google Scholar
Google Scholar
[20] Kim H T, Jeong O C 2011 Microelectron. Eng. 88 2281
 Google Scholar
Google Scholar
[21] Borók A, Laboda K, Bonyár A 2021 Biosensors-Basel 11 292
 Google Scholar
Google Scholar
[22] Kratz S R A, Bachmann B, Spitz S, Höll G, Eilenberger C, Goeritz H, Ertl P, Rothbauer M 2020 Sci. Rep. 10 1400
 Google Scholar
Google Scholar
[23] Xiong L, Chen P, Zhou Q 2014 J. Adhes. Sci. Technol. 28 1046
 Google Scholar
Google Scholar
[24] Ouellet E, Yang C W, Lin T, Yang L L, Lagally E T 2010 Langmuir 26 11609
 Google Scholar
Google Scholar
[25] Rashidi H, Alhaque S, Szkolnicka D, Flint O, Hay D C 2016 Arch. Toxicol. 90 1757
 Google Scholar
Google Scholar
[26] Kimura H, Nishikawa M, Yanagawa N, Nakamura H, Miyamoto S, Hamon M, Hauser P, Zhao L, Jo O D, Komeya M, Ogawa T, Yanagawa N 2018 Biomicrofluidics 12 044107
 Google Scholar
Google Scholar
[27] Qamar M I, Read A E 1987 Gut 28 583
 Google Scholar
Google Scholar
[28] Takahashi T 2011 J. Nutr. Sci. Vitaminol. 57 265
 Google Scholar
Google Scholar
[29] Paszkowiak J J, Dardik A 2003 Vasc. Endovas. Surg. 37 47
 Google Scholar
Google Scholar
[30] van Haaften E E, Wissing T B, Rutten M C M, Bulsink J A, Gashi K, van Kelle M A J, Smits A, Bouten C V C, Kurniawan N A 2018 Tissue Eng. Part C 24 418
 Google Scholar
Google Scholar
[31] Morinaga K, Okadome K, Kuroki M, Miyazaki T, Muto Y, Inokuchi K 1985 J. Vasc. Surg. 2 430
 Google Scholar
Google Scholar
[32] Koutsiaris A G, Tachmitzi S V, Batis N 2013 Microvasc. Res. 85 34
 Google Scholar
Google Scholar
[33] Tan H Y, Trier S, Rahbek U L, Dufva M, Kutter J P, Andresen T L 2018 PLoS One 13 e0197101
 Google Scholar
Google Scholar
[34] Delon L C, Guo Z, Oszmiana A, Chien C-C, Gibson R, Prestidge C, Thierry B 2019 Biomaterials 225 119521
 Google Scholar
Google Scholar
[35] Chi M, Yi B, Oh S, Park D, Sung J H, Park S 2015 Biomed. Microdevices 17 9966
 Google Scholar
Google Scholar
[36] Sakharov D, Maltseva D, Knyazev E, Nikulin S, Poloznikov A, Shilin S, Baranova A, Tsypina I, Tonevitsky A 2019 BMC Syst. Biol. 13 19
 Google Scholar
Google Scholar
[37] Strelnikova N, Herren F, Schoenenberger C A, Pfohl T 2016 Front. Mater. 3 20
 Google Scholar
Google Scholar
[38] Spuul P, Chi P Y, Billottet C, Chou C F, Génot E 2016 Methods 94 65
 Google Scholar
Google Scholar
[39] Cheng M, Guan X, Li H, Cui X, Zhang X, Li X, Jing X, Wu H, Avsar E 2013 PLoS One 8 e67675
 Google Scholar
Google Scholar
[40] Manevich E, Grabovsky V, Feigelson S W, Alon R 2007 J. Biol. Chem. 282 25338
 Google Scholar
Google Scholar
-
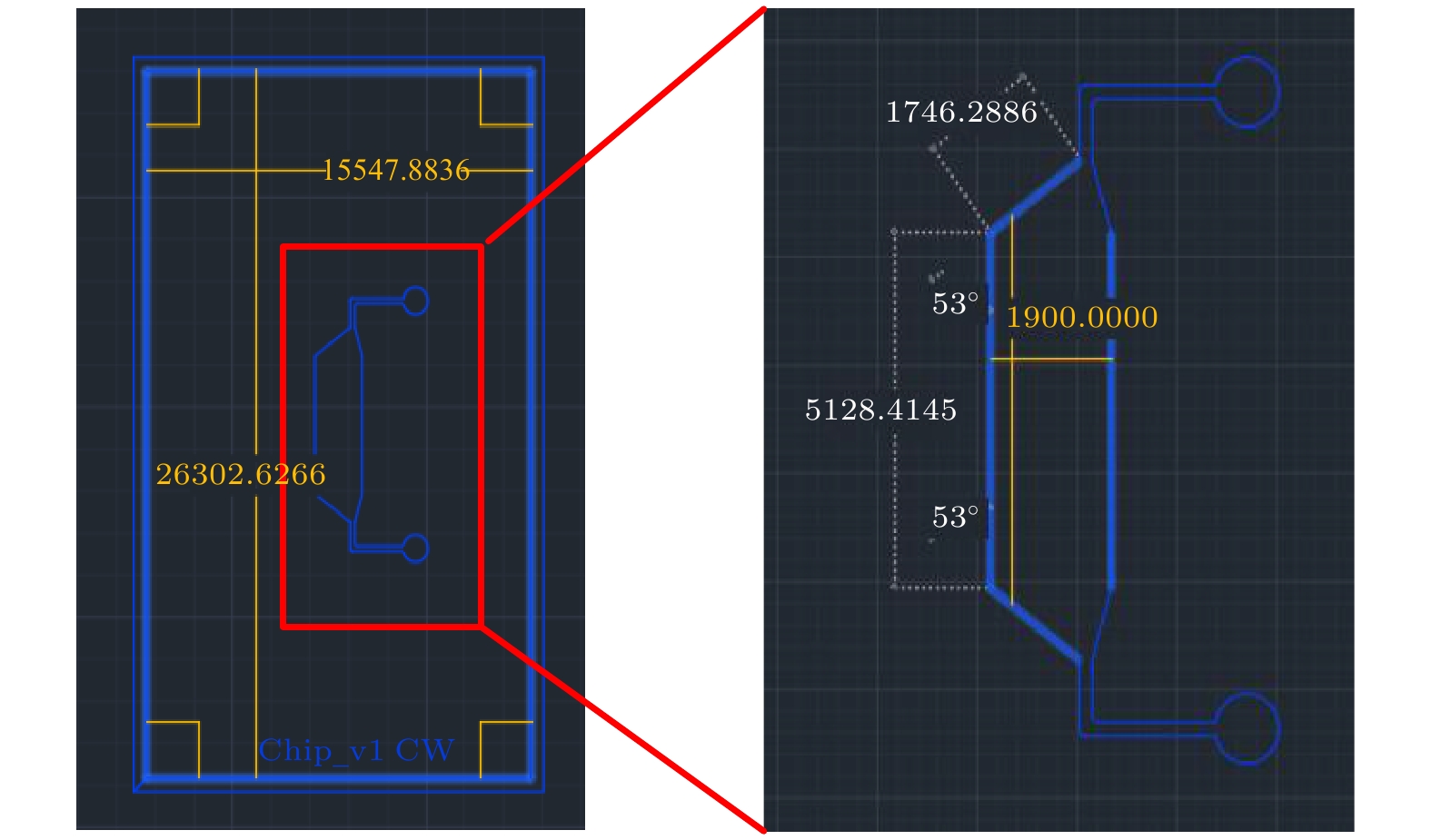
图 1 COP-PDMS共键合微流控芯片倒模制作图例 (a) 通过光刻技术形成以SU-8和硅片为基底的圆形微流控芯片阵列式模具; (b) 切割后的单个微流控芯片模块; (c) PDMS模块与COP板材通过等离子处理后键合; (d) 在形成的COP-PDMS微流控沟道中进行动态细胞培养的侧面图; (e) 含有细胞的微流控沟道的三维图
Fig. 1. Schematic fabrication process of COP-PDMS co-bonded microfluidic device: (a) Using soft lithography technology to prepare the round microfluidic device array mold on the SU-8 and silicon wafer; (b) the single microfluidic device module; (c) the PDMS module and COP plate are fabricated by plasma treatment; (d) side view of cells dynamically cultured in the COP-PDMS microfluidic channel; (e) three-dimensional view of microfluidic channels containing cells.
图 3 (a) 键合过程加压后(0至5000 Pa) COP-PDMS微流控芯片的键合强度测试结果, 键合强度代表的是完全剥离两种材料需要的剪切应力, 该剪切应力通过推拉力计测量得出; (b) 芯片键合强度与额外加压的对应关系; (c) 高灌注速率(200 μL/s)下沟道变形及密封度变化情况; (d) 2 周长时程动态灌注(灌注速率为0.05 μL/s)后沟道形变及密封度变化情况
Fig. 3. (a) Bonding strength test results of COP-PDMS microfluidic device with the vary compressions (0 to 5000 Pa) during the bonding process. The bonding strength represents the shear stress required for completely stripping two materials, which is measured by push-tension meter. (b) The corresponding relationship between the bonding strength of microfluidic device and the compressions during the bonding process. (c) The seal and deformation change of channels and chamber at high fluid perfusion rate (200 μL/s). (d) The seal and deformation change of channels and chamber after a 2-week time-course dynamic perfusion (0.05 μL/s)
图 A3 在COP-PDMS微流控芯片中动态和静态培养中, Caco-2细胞的ZO-1, Paxillin和F-actin的免疫荧光检测(图中基准尺为20 μm) (a) ZO-1与F-actin的免疫荧光染色; (b) Paxillin与F-actin的免疫荧光染色; (c) 对(a)和(b)图中太赫兹辐照前后ZO-1, Paxillin和F-actin免疫荧光强度定量分析结果(t检验显著性差异: p < 0.05, *; p < 0.01, **)
Fig. A3. Immunofluorescence staining results of Caco-2 cells that are dynamically and statically cultured in COP-PDMS microfluidic device (scale bar: 20 μm). (a) The confocal result of ZO-1 and F-actin. (b) The confocal result of Paxillin and F-actin. (c) Quantitative analysis of immunofluorescence intensity of ZO-1, Paxillin and F-actin of the cells in panel (a) and (b): The quantification is determined as immunofluorescence intensity corresponding to 104 nuclei (significance of t-test: p < 0.05, *; p < 0.01, **).
图 4 太赫兹辐照对COP-PDMS微流控芯片中动态培养的Caco-2细胞的ZO-1, Paxillin和F-actin的免疫荧光检测(图中基准尺为20 μm) (a) ZO-1与F-actin的免疫荧光染色; (b) Paxillin与F-actin的免疫荧光染色; (c) 对(a)和(b)图中太赫兹辐照前后ZO-1, Paxillin和F-actin免疫荧光强度定量分析结果(t检验显著性差异: p < 0.05, *; p < 0.01, **)
Fig. 4. Immunofluorescence staining results of Caco-2 cells that are dynamically cultured in COP-PDMS microfluidic device, before and after terahertz irradiation (scale bar: 20 μm). (a) The confocal result of ZO-1 and F-actin. (b) The confocal result of Paxillin and F-actin. (c) Quantitative analysis of immunofluorescence intensity of ZO-1, Paxillin and F-actin of the cells in panel (a) and (b): The quantification is determined as immunofluorescence intensity corresponding to 104 nuclei (significance of t-test: p < 0.05, *; p < 0.01, **).
表 1 生物体内各个组织器官中的流体剪切应力及在COP-PDMS微流控芯片中模拟对应流体剪切应力需要的流体流量
Table 1. Shearing stress in the in-vivo tissues and the corresponding fluidic perfusion rate in the COP-PDMS microfluidic device to simulate the shearing stress.
-
[1] Fröhlich H 1975 Proc. Natl. Acad. Sci. U. S. A. 72 4211
 Google Scholar
Google Scholar
[2] Smye S W, Chamberlain J M, Fitzgerald A J, Berry E 2001 Phys. Med. Biol. 46 R101
 Google Scholar
Google Scholar
[3] Qin J, Ying Y, Xie L 2013 Appl. Spectrosc. Rev. 48 439
 Google Scholar
Google Scholar
[4] Greschner A A, Ropagnol X, Kort M, Zuberi N, Perreault J, Razzari L, Ozaki T, Gauthier M A 2019 J. Am. Chem. Soc. 141 3456
 Google Scholar
Google Scholar
[5] Yamazaki S, Harata M, Idehara T, Konagaya K, Yokoyama G, Hoshina H, Ogawa Y 2018 Sci. Rep. 8 9990
 Google Scholar
Google Scholar
[6] Titova L V, Ayesheshim A K, Golubov A, Fogen D, Rodriguez-Juarez R, Hegmann F A, Kovalchuk O 2013 Biomed. Opt. Express 4 559
 Google Scholar
Google Scholar
[7] Olshevskaya J S, Kozlov A, Petrov A K, Zapara T A, Ratushnyak A 2010 Vestn. Novosib. State Univ. Ser. Phys. 5 185
[8] Alfihed S, Holzman J F, Foulds I G 2020 Biosens. Bioelectron. 165 112393
 Google Scholar
Google Scholar
[9] Naftaly M, Gregory A 2021 Appl. Sci. 11 6733
 Google Scholar
Google Scholar
[10] Cunningham P, Valdes N, Vallejo F, Hayden L, Polishak B, Zhou X H, Luo J, Jen A, Williams J, Twieg R 2011 J. Appl. Phys. 109 043505
 Google Scholar
Google Scholar
[11] Alfihed S, Bergen M H, Ciocoiu A, Holzman J F, Foulds I G 2018 Micromachines-Basel 9 E453
 Google Scholar
Google Scholar
[12] Cheng C, Zhu Z, Li S, Ren G, Zhang J, Cong H, Peng Y, Han J, Chang C, Zhao H 2019 RSC Adv. 9 20240
 Google Scholar
Google Scholar
[13] George P A, Hui W, Rana F, Hawkins B G, Smith A E, Kirby B J 2008 Opt. Express 16 1577
 Google Scholar
Google Scholar
[14] Wang C, Dang T, Baste J, Joshi A A, Bhushan A 2021 FASEB J. 35 e21291
 Google Scholar
Google Scholar
[15] Wang C, Tanataweethum N, Karnik S, Bhushan A 2018 ACS Biomater. Sci. Eng. 4 1377
 Google Scholar
Google Scholar
[16] Xu B Y, Yan X N, Xu J J, Chen H Y 2012 Biomicrofluidics 6 16507
 Google Scholar
Google Scholar
[17] Jang K J, Mehr A P, Hamilton G A, McPartlin L A, Chung S, Suh K Y, Ingber D E 2013 Integr. Biol. 5 1119
 Google Scholar
Google Scholar
[18] Kim S W, Ehrman J, Ahn M R, Kondo J, Lopez A A M, Oh Y S, Kim X H, Crawley S W, Goldenring J R, Tyska M J, Rericha E C, Lau K S 2017 Mol. Biol. Cell 28 3043
 Google Scholar
Google Scholar
[19] D'Angelo F, Mics Z, Bonn M, Turchinovich D 2014 Opt. Express 22 12475
 Google Scholar
Google Scholar
[20] Kim H T, Jeong O C 2011 Microelectron. Eng. 88 2281
 Google Scholar
Google Scholar
[21] Borók A, Laboda K, Bonyár A 2021 Biosensors-Basel 11 292
 Google Scholar
Google Scholar
[22] Kratz S R A, Bachmann B, Spitz S, Höll G, Eilenberger C, Goeritz H, Ertl P, Rothbauer M 2020 Sci. Rep. 10 1400
 Google Scholar
Google Scholar
[23] Xiong L, Chen P, Zhou Q 2014 J. Adhes. Sci. Technol. 28 1046
 Google Scholar
Google Scholar
[24] Ouellet E, Yang C W, Lin T, Yang L L, Lagally E T 2010 Langmuir 26 11609
 Google Scholar
Google Scholar
[25] Rashidi H, Alhaque S, Szkolnicka D, Flint O, Hay D C 2016 Arch. Toxicol. 90 1757
 Google Scholar
Google Scholar
[26] Kimura H, Nishikawa M, Yanagawa N, Nakamura H, Miyamoto S, Hamon M, Hauser P, Zhao L, Jo O D, Komeya M, Ogawa T, Yanagawa N 2018 Biomicrofluidics 12 044107
 Google Scholar
Google Scholar
[27] Qamar M I, Read A E 1987 Gut 28 583
 Google Scholar
Google Scholar
[28] Takahashi T 2011 J. Nutr. Sci. Vitaminol. 57 265
 Google Scholar
Google Scholar
[29] Paszkowiak J J, Dardik A 2003 Vasc. Endovas. Surg. 37 47
 Google Scholar
Google Scholar
[30] van Haaften E E, Wissing T B, Rutten M C M, Bulsink J A, Gashi K, van Kelle M A J, Smits A, Bouten C V C, Kurniawan N A 2018 Tissue Eng. Part C 24 418
 Google Scholar
Google Scholar
[31] Morinaga K, Okadome K, Kuroki M, Miyazaki T, Muto Y, Inokuchi K 1985 J. Vasc. Surg. 2 430
 Google Scholar
Google Scholar
[32] Koutsiaris A G, Tachmitzi S V, Batis N 2013 Microvasc. Res. 85 34
 Google Scholar
Google Scholar
[33] Tan H Y, Trier S, Rahbek U L, Dufva M, Kutter J P, Andresen T L 2018 PLoS One 13 e0197101
 Google Scholar
Google Scholar
[34] Delon L C, Guo Z, Oszmiana A, Chien C-C, Gibson R, Prestidge C, Thierry B 2019 Biomaterials 225 119521
 Google Scholar
Google Scholar
[35] Chi M, Yi B, Oh S, Park D, Sung J H, Park S 2015 Biomed. Microdevices 17 9966
 Google Scholar
Google Scholar
[36] Sakharov D, Maltseva D, Knyazev E, Nikulin S, Poloznikov A, Shilin S, Baranova A, Tsypina I, Tonevitsky A 2019 BMC Syst. Biol. 13 19
 Google Scholar
Google Scholar
[37] Strelnikova N, Herren F, Schoenenberger C A, Pfohl T 2016 Front. Mater. 3 20
 Google Scholar
Google Scholar
[38] Spuul P, Chi P Y, Billottet C, Chou C F, Génot E 2016 Methods 94 65
 Google Scholar
Google Scholar
[39] Cheng M, Guan X, Li H, Cui X, Zhang X, Li X, Jing X, Wu H, Avsar E 2013 PLoS One 8 e67675
 Google Scholar
Google Scholar
[40] Manevich E, Grabovsky V, Feigelson S W, Alon R 2007 J. Biol. Chem. 282 25338
 Google Scholar
Google Scholar
计量
- 文章访问数: 12215
- PDF下载量: 181
- 被引次数: 0













 下载:
下载: